
Obstructive Sleep Apnea
Obstructive sleep apnea is a serious medical disorder seen primarily in men. Unfortunately, this is frequent overlooked as “normal” snoring. This condition occurs when obstructions in the nose and throat block the ability to breathe.
This can cause several symptoms including:
- Gasping for air during sleep
- Witnessed apnea (stopping of breathing for at least 10 seconds)
- Waking up tired, even after a full night’s sleep
- Feeling sleepy during the day (at work or while driving)
- Irritability or short temper
- Problems with concentration or memory
- Medical conditions such as high blood pressure and heart disease
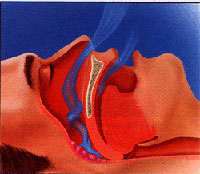
Breathing During Sleep
Snoring is caused when there is narrowing of the normal airway. Because of a phenomenon known as the “Bernoulli Effect”, air flows faster through a narrowed passage similar to how water sprays faster and farther when you put your finger on the tip of a garden hose.
This faster flow of air causes high frequency vibrations of the soft tissue of the airway resulting in the characteristic sounds of snoring.
Different patterns and sounds of snoring can occur if the obstruction is located in the nose or in the back of the throat.
Obstructive sleep apnea occurs when there is an actual obstruction of airflow and no air enters the lungs. This usually occurs during deep sleep due to relaxation of the muscles of the throat that keep the airway open during the day. The body sense the inability to breathe and tries to open the airway by bringing the brain out of deep sleep to restore muscle tone and the airway (gasping and frequent arousals at night). Given the choice between deep, restful sleep and oxygen, the body chooses oxygen. The resultant disruption and lack of deep, restful sleep results in the brain craving sleep during the day (feeling tired or even falling asleep during quite periods)
 If left untreated, obstructive sleep apnea can lead to serious health and
safety consequences. There is an increased risk of automobile accidents
because of the impaired concentration and attention deficit that is caused
by the apnea. In fact, the risk is the same as if one had three drinks
before driving every time one gets behind the wheel! Long term risks include
high blood pressure, heart disease, heart attack, stroke and sudden death.
This is not a small risk. One study show that over 50% (!) of men with
untreated obstructive sleep apnea suffer a serious health condition or
even death within 10 years.
If left untreated, obstructive sleep apnea can lead to serious health and
safety consequences. There is an increased risk of automobile accidents
because of the impaired concentration and attention deficit that is caused
by the apnea. In fact, the risk is the same as if one had three drinks
before driving every time one gets behind the wheel! Long term risks include
high blood pressure, heart disease, heart attack, stroke and sudden death.
This is not a small risk. One study show that over 50% (!) of men with
untreated obstructive sleep apnea suffer a serious health condition or
even death within 10 years.
The doctor will perform a detailed history and physical examination including an endoscopic examination of the upper airway. He will also recommend a sleep study (overnight polysomnography) to objectively quantitate the severity of the disease. Based on his finding, he will recommend one of several treatment options.
Treatment for Obstructive Sleep Apnea
There are four major treatment regimens for obstructive sleep apnea.
The first involves weight loss, avoidance of sedatives (including alcohol, antihistamines and sleep aids), and avoidance of sleeping on one’s back. Although this is simplest treatment option, it often does not correct the problem.
The second option is CPAP, or Continuous Positive Airway Pressure. This involves wearing a mask at night that attached to an air blower. A gentle, steady stream of air through the nose and throat keeps the airway structures from collapsing and thus prevents obstruction of breathing. The pressure is customized to your needs but has to be used every night to be effective. CPAP offers a high degree of success in treatment and avoids surgery. However, it may be uncomfortable or patients may not be willing to wear a mask every night or during travel.
The third option is utilizing oral appliances to keep the tongue and/or the jaw forward to prevent airway collapse. Sleep strips on the nose may also help improve the nasal airway. Consultation with a dentist who specializes in these appliances can help fashion the most appropriate appliances for the individual.
The fourth option is surgery to improve the airway in the nose and throat.
 A septoplasty to fix a deviated nasal septum will improve breathing through
the nose. Incisions are made inside the nose and there is usually no bruising
or swelling on the outside of the nose. Septal bone and cartilage are
straightened to allow air to flow freely through the nose.
A septoplasty to fix a deviated nasal septum will improve breathing through
the nose. Incisions are made inside the nose and there is usually no bruising
or swelling on the outside of the nose. Septal bone and cartilage are
straightened to allow air to flow freely through the nose.
Reduction of the turbinates (soft tissue located opposite the septum) may also be shrunk to improve the airway. A combination of these procedures results in a larger diameter for the nasal air passage and improved flow. Physics state that laminar flow is a 5th power exponential function of radius. In simple terms, that means if the radius (or width) of the nasal passage is doubled, airflow will increase 32-fold! Usually, the improvement is not that dramatic, but this illustrates why even a slight enlargement of the nasal passage will have beneficial effects on nasal breathing.
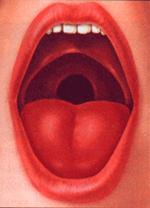 Tissue in the back of throat may also be “trimmed” to prevent
large, floppy tissue from obstructing the airway. Subsequent healing contracture
after surgery will also stiffen the tissues so they are not so floppy.
The uvula (the “punching bag hanging from the roof of your mouth),
the back free edge of the roof of your mouth, the tonsils (if present)
and the the side walls of the back of your mouth will be trimmed in a
procedure called UPPP (UvuloPalatoPharyngoPlasty).
Tissue in the back of throat may also be “trimmed” to prevent
large, floppy tissue from obstructing the airway. Subsequent healing contracture
after surgery will also stiffen the tissues so they are not so floppy.
The uvula (the “punching bag hanging from the roof of your mouth),
the back free edge of the roof of your mouth, the tonsils (if present)
and the the side walls of the back of your mouth will be trimmed in a
procedure called UPPP (UvuloPalatoPharyngoPlasty).
This procedure is painful (for about two weeks) and is performed in a hospital. The success rate is slightly lower than CPAP. The upside is that, if successful, no further intervention may be required.
In addition to these procedures, the doctor may also perform a tongue base suspension. The back of the tongue is also a structure which can collapse into the airway. A simple sling of thin but strong suture, anchored to the inside of the jaw bone, is placed underneath the lining of the floor of the mouth and tongue. This is usually not noticeable during the day and, at night, prevents the tongue from falling back into the airway.
Obstructive sleep apnea is a serious disease which requires prompt examination and testing.
-
ENT/Otolaryngology ENT, Otolaryngology 2557 Mowry Ave.
Suite 30
Fremont, CA 94538
(510) 248-1590 More Information




